What is PRP treatment for
Chronic Pain & Sport Injuries?
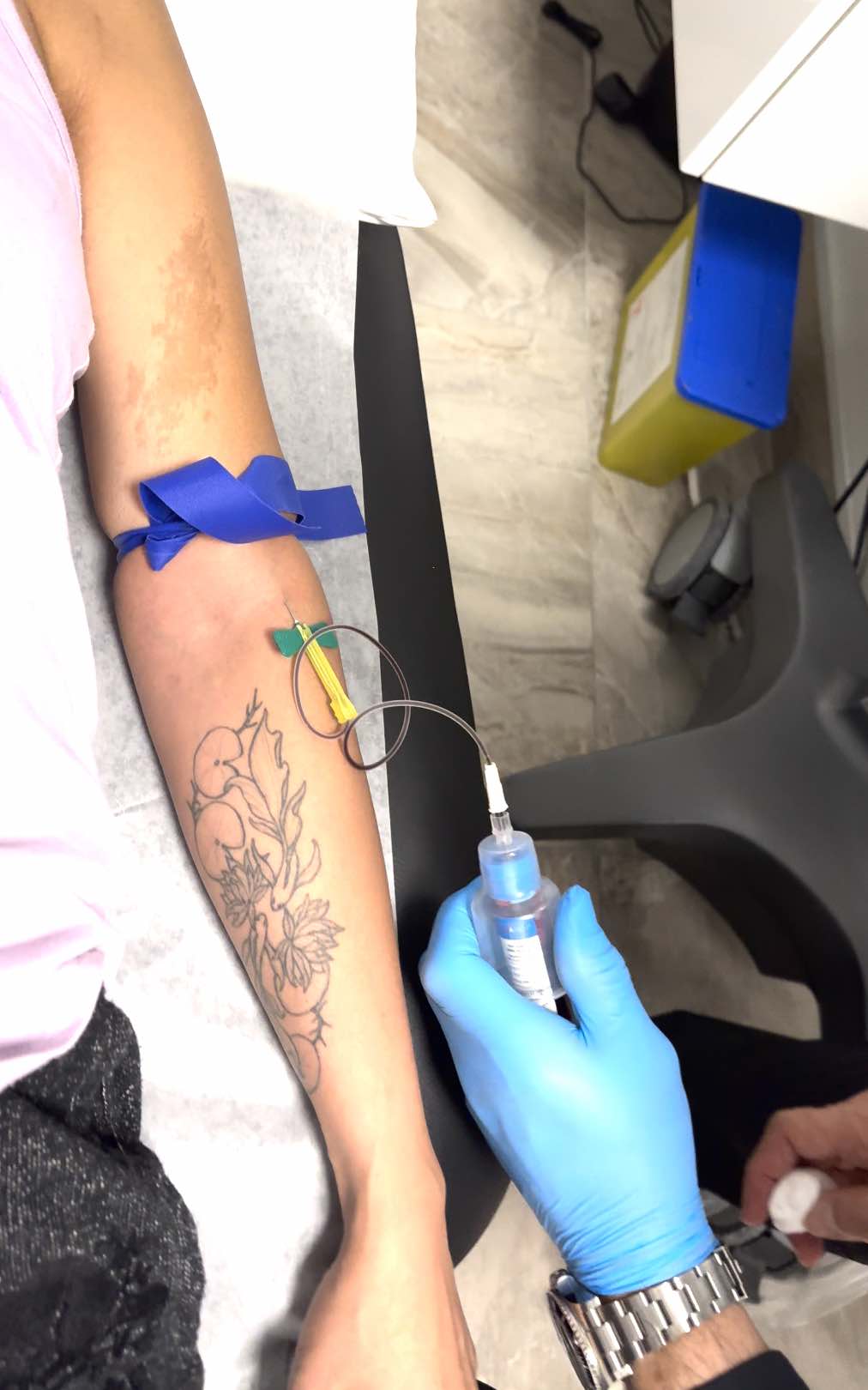
Platelet-Rich Plasma (PRP) therapy is a regenerative treatment that harnesses your body's natural healing abilities to repair damaged tissues and reduce pain. This advanced therapy involves drawing a small sample of your blood, processing it in a centrifuge to concentrate the platelets, and injecting the platelet-rich plasma into injured tendons, ligaments, muscles, bones, or joints.
PRP is widely used to treat sports injuries, chronic pain, and musculoskeletal conditions, helping to accelerate tissue repair and reduce inflammation. By enhancing the body's natural healing response, PRP treatments in Richmond Hill may minimize reliance on pain medications and promote long-term recovery. Whether you're struggling with joint pain, tendon injuries, or mobility issues, PRP therapy offers a non-surgical solution to restore function and improve quality of life.