what is Achondroplasia?
Achondroplasia is a genetic disorder causing short-limb dwarfism due to improper cartilage development in the arms and legs. It results from a mutation in the FGFR3 gene, which disrupts normal bone growth. Adults with achondroplasia typically reach heights of 42 to 56 inches.
This condition can also lead to neurological issues in 20 to 50 percent of affected children. Managing achondroplasia involves genetic counseling and medical care to address related health concerns.
What is the difference between achondroplasia and skeletal dysplasia (dwarfism)?
Achondroplasia is the most common form of skeletal dysplasia, which is the umbrella term used to identify hundreds of conditions that affect the growth of bones and cartilage. Achondroplasia specifically targets bone growth in your arms and legs.
Is achondroplasia hereditary?
Most cases of achondroplasia are not inherited. Anyone can be affected by achondroplasia. Around 80% of individuals with achondroplasia have parents of normal height and are born with a new gene alteration (de novo mutation). It is rare that these parents will have another child with achondroplasia.
Only one parent needs to pass down the gene for a child to be born with achondroplasia (autosomal dominant). There is a 50% chance of a person with achondroplasia and a partner who does not have achondroplasia having a child with the disorder.
If both parents have achondroplasia, there is a 25% chance that the child will be born with homozygous achondroplasia, which leads to stillbirth or death shortly after birth.
Symptoms
Achondroplasia, a genetic disorder, manifests through a variety of physical characteristics and developmental delays. Common symptoms include:
- Shortened Limbs: Upper arms and thighs are more affected than forearms and lower legs.
- Large Head Size: Prominent forehead and flattened nasal bridge.
- Dental Issues: Crowded or misaligned teeth.
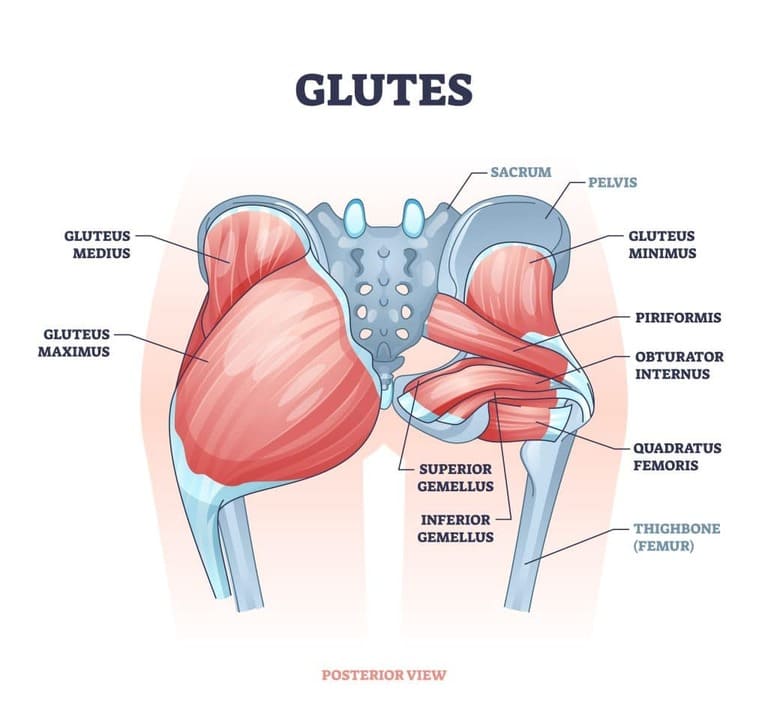
- Spinal Abnormalities: Curved lower spine (lordosis) which may lead to kyphosis (a small hump near the shoulders).
- Small Vertebral Canals: Potential for spinal cord compression during adolescence.
- Bowed Legs: Noticeable curvature in lower legs.
- Flat, Broad Feet: Often accompanied by shortness.
- Trident Hand: Extra space between the middle and ring fingers.
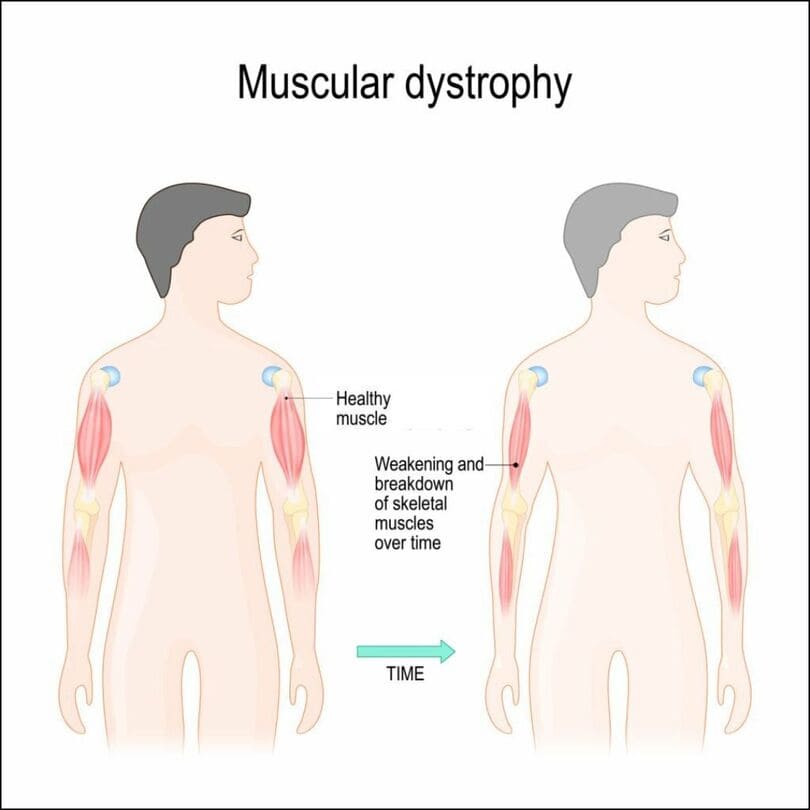
- Muscle and Joint Issues: Poor muscle tone and loose joints.
- Ear Infections: Frequent middle ear infections that may lead to hearing loss.
- Developmental Delays: Delays in milestones like walking, which may occur between 18 to 24 months instead of around 12 months.
- Respiratory Problems: Issues such as obstructive sleep apnea.
- Hydrocephalus: Excess fluid on the brain.
Causes
Achondroplasia is caused by a mutation in the FGFR3 gene, which affects the conversion of cartilage to bone during fetal development. This mutation leads to shortened and abnormally shaped bones, resulting in the characteristic features of the condition.
Diagnosis and Tests
Achondroplasia can be diagnosed both before and after birth through a series of medical assessments and tests.
Diagnosis
Achondroplasia can often be detected before birth using fetal ultrasound, particularly when the baby exhibits shorter-than-average limbs and a larger head size. However, confirmation typically occurs after birth through:
- Physical Examination: A thorough examination to assess physical characteristics associated with achondroplasia.
- X-ray: Imaging to visualize bone abnormalities.
- Genetic Testing: Identification of the FGFR3 gene mutation.
- MRI or CT Scan: Used to evaluate potential complications such as muscle weakness or spinal cord compression.
Tests
- Prenatal Ultrasound: Enables early detection of skeletal abnormalities.
- DNA Testing: Offers confirmation before birth, especially for parents with heightened risk factors.
These diagnostic approaches ensure accurate identification of achondroplasia, facilitating appropriate medical management and support from an early stage.
Management and Treatment
Managing achondroplasia focuses on symptom monitoring and addressing complications rather than curing the condition.
Monitoring and Assessment: Close monitoring in infancy and regular evaluations throughout childhood to detect and manage complications early.
Diagnostic Imaging: X-rays, MRI scans for spinal stenosis, and CT scans for vertebrae assessment.
Surgical Interventions: May include decompression and fusion surgeries for severe spinal issues or limb correction procedures.
Specialized Procedures: Ventriculoperitoneal shunt for managing hydrocephalus.
Supportive Care: Includes weight management, healthy diet, and treatments for ear infections and sleep apnea.
Growth Hormone Therapy: Some individuals may benefit to optimize growth potential.
Social Support: Encouragement of socialization and emotional support for individuals and families.
While achondroplasia cannot be cured, proactive management and interventions enhance quality of life and reduce potential complications associated with the condition.
Conclusion
In conclusion, while achondroplasia cannot be cured, proactive management and timely interventions are key to improving the quality of life for individuals affected by this genetic condition. Regular monitoring, surgical options for severe cases, supportive care, and ongoing research offer hope for better outcomes and enhanced understanding in the future. With proper medical guidance and support from healthcare providers, individuals with achondroplasia can navigate the challenges associated with the condition and lead fulfilling lives.