Introduction:
Arthritis is a common and often painful condition that affects millions of individuals worldwide. It’s not a single disease but rather a group of more than 100 different types of joint-related conditions. In this comprehensive article, we will delve into Arthritis, exploring its causes, symptoms, effective treatment options, including the crucial roles of physiotherapy and osteopathy. We’ll also touch on related diseases and provide valuable insights for managing this condition.
Understanding Arthritis:
Arthritis is a complex and multifaceted health challenge that primarily affects the joints. These vital connectors in our bodies allow for movement, but when afflicted by arthritis, they can become sources of chronic pain and discomfort. It’s essential to recognize that arthritis doesn’t discriminate – it can affect individuals of all ages, genders, and backgrounds.
The Complexity of Arthritis:
The term Arthritis encompasses a wide array of conditions, each with its unique characteristics. Among the most common forms are osteoarthritis and rheumatoid arthritis. Osteoarthritis, often associated with the wear and tear of joints over time, is a leading cause of pain and mobility issues in older adults. Rheumatoid arthritis, on the other hand, is an autoimmune disorder where the body’s immune system mistakenly attacks the joints, leading to inflammation and pain.
Causes of Arthritis:
Arthritis is a multifaceted condition with various underlying causes, and understanding these triggers is essential for effective management. Here, we delve deeper into the key factors contributing to arthritis:
Age and Wear and Tear: Osteoarthritis, the most prevalent form of arthritis, often develops with age as joint tissues naturally degenerate over time. Repetitive use and wear and tear on joints can accelerate this process.
Genetics: Family history plays a significant role in some forms of arthritis. If close relatives have arthritis, there may be a genetic predisposition that increases the risk of developing the condition.
Autoimmune Responses: Rheumatoid arthritis and other autoimmune forms of arthritis occur when the body’s immune system mistakenly attacks healthy joint tissues. These conditions are characterized by chronic inflammation and joint damage.
Infections: In rare cases, infections can trigger reactive arthritis. Bacterial or viral infections elsewhere in the body can lead to joint inflammation.
Metabolic Abnormalities: Conditions like gout result from metabolic abnormalities, particularly elevated levels of uric acid in the bloodstream. This excess uric acid can crystallize in joints, causing intense pain and inflammation.
Symptoms of Arthritis:
Arthritis presents a wide spectrum of symptoms that can significantly impact an individual’s daily life. Recognizing these signs is crucial for early diagnosis and effective management. Here, we outline the common symptoms associated with arthritis:
Joint Pain: Persistent and often severe joint pain is a hallmark of arthritis. The pain can range from a dull ache to sharp, shooting sensations and may be more pronounced during movement.
Joint Swelling: Inflammation of the joints leads to swelling, which can be visibly apparent and cause joint deformities over time.
Stiffness: Arthritis-related stiffness can make it challenging to initiate movement, particularly after periods of inactivity, such as waking up in the morning.
Limited Range of Motion: Reduced flexibility and range of motion in affected joints can hinder daily activities like bending, reaching, or walking.
Fatigue: Many individuals with arthritis experience fatigue, often attributed to the body’s constant battle against inflammation.
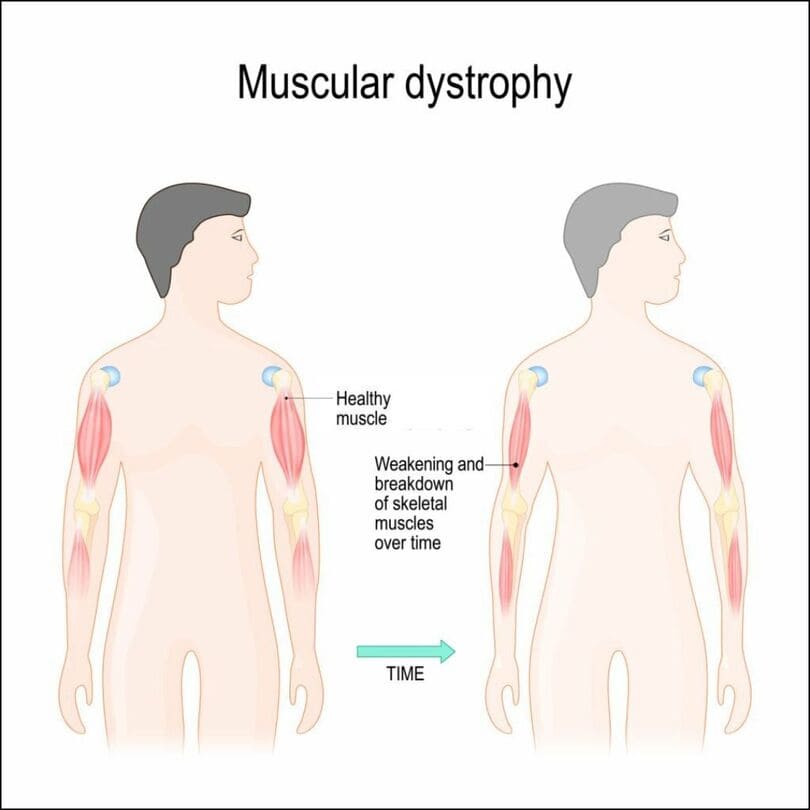
Weakness: Muscles around affected joints may weaken due to reduced use, leading to further functional limitations.
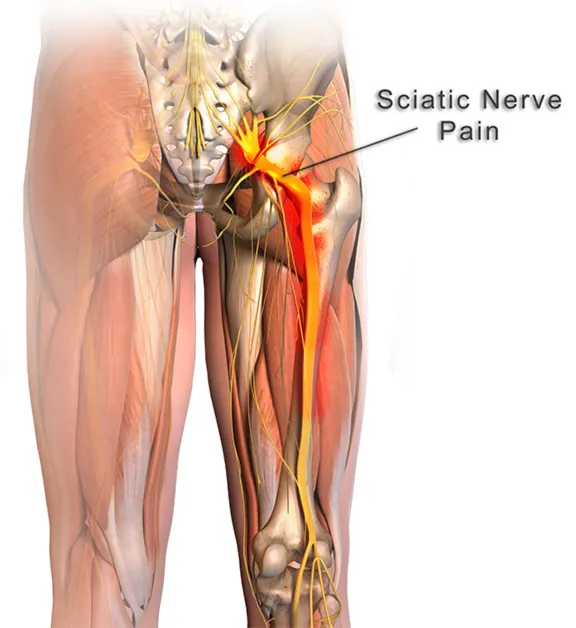
Numbness and Tingling: In some cases, nerve compression or irritation related to arthritis can result in sensations of numbness or tingling in the hands or feet.
Fever and Weight Loss: Systemic symptoms like fever and unexplained weight loss can accompany certain forms of inflammatory arthritis.
Joint Warmth and Redness: Inflammation can cause affected joints to become warm to the touch and appear red or flushed.
It’s crucial to remember that the severity and combination of these symptoms can vary widely among individuals and arthritis types. Early consultation with healthcare professionals and a tailored treatment plan, which may include physiotherapy and osteopathy, can significantly improve one’s quality of life when living with arthritis.
Types of Arthritis:
Arthritis isn’t a single, uniform condition; it encompasses a diverse group of disorders, each with its unique characteristics and underlying causes. Understanding the various types of arthritis is essential for accurate diagnosis and effective management. Here, we explore some of the most prevalent types:
- Osteoarthritis (OA): Osteoarthritis is the most common form of arthritis, typically associated with the natural aging process. It occurs as the protective cartilage that cushions the ends of bones deteriorates over time. OA commonly affects weight-bearing joints like the knees, hips, and spine, causing pain, stiffness, and reduced mobility.
- Rheumatoid Arthritis (RA): Rheumatoid arthritis is an autoimmune disorder in which the body’s immune system mistakenly attacks the synovium—the lining of the membranes that surround the joints. This leads to chronic inflammation, joint damage, and pain. RA often affects joints on both sides of the body, such as wrists, knees, and fingers.
- Psoriatic Arthritis: Psoriatic arthritis is a type of inflammatory arthritis that occurs in individuals with psoriasis, a skin condition characterized by red, scaly patches. It can affect any joint and may involve the fingers and toes, causing swelling, pain, and stiffness.
- Ankylosing Spondylitis: Ankylosing spondylitis primarily affects the spine and sacroiliac joints, leading to chronic inflammation and pain. Over time, it can cause the vertebrae to fuse, resulting in reduced mobility. This condition often starts in early adulthood and disproportionately affects men.
- Gout: Gout is caused by the buildup of uric acid crystals in the joints, resulting in sudden and severe joint pain, often in the big toe. Dietary factors and genetics play a role in its development. Gout flares can be managed with medications and lifestyle changes.
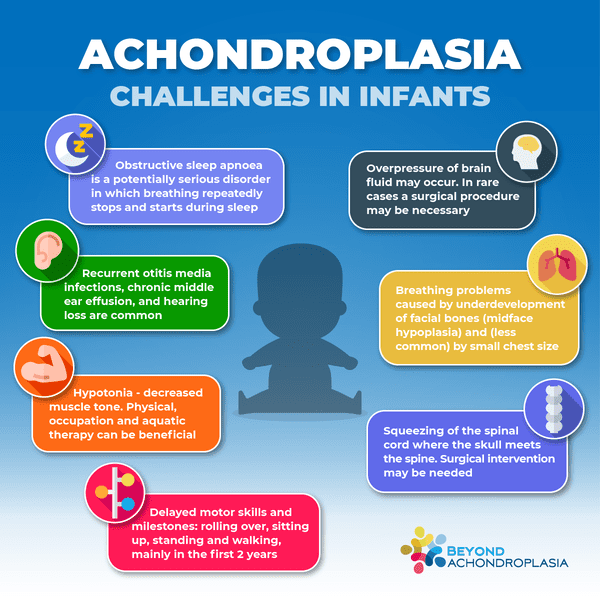
- Juvenile Arthritis: Juvenile arthritis refers to a group of autoimmune disorders that affect children under the age of 16. The most common form is juvenile idiopathic arthritis (JIA), which causes joint inflammation, pain, and stiffness. Early diagnosis and treatment are crucial to prevent long-term joint damage.
- Lupus (Systemic Lupus Erythematosus): While primarily known as a systemic autoimmune disease, lupus can also manifest as a form of inflammatory arthritis. It can affect multiple organs and joints, leading to pain, swelling, and fatigue.
- Septic Arthritis: Septic arthritis is a bacterial or fungal joint infection, typically caused by the spread of infection from another part of the body. It leads to sudden joint pain, swelling, and fever. Prompt medical attention is essential to prevent joint damage.
- Reactive Arthritis: Reactive arthritis is triggered by infections, typically in the gastrointestinal or genitourinary tract. It can cause joint pain, swelling, and inflammation, along with other symptoms like eye or skin irritation.
- Fibromyalgia: While not classified as a traditional arthritis, fibromyalgia shares common symptoms with some forms of arthritis, such as chronic pain and fatigue. It primarily affects the muscles and soft tissues, leading to widespread pain and tenderness.
- Thumb Arthritis (Basal Joint Arthritis):
Thumb arthritis, also known as basal joint arthritis, is a specific type of osteoarthritis that affects the base of the thumb. This condition typically arises due to the wear and tear of the joint over time.
Understanding the specific type of arthritis an individual has is crucial for tailoring treatment approaches effectively. A healthcare provider’s diagnosis and comprehensive evaluation are key steps in managing arthritis and improving overall quality of life.
Holistic Approaches to Treatment:
Effectively managing arthritis requires a comprehensive approach. While medications can help alleviate pain and inflammation, physiotherapy and osteopathy play pivotal roles in improving an individual’s quality of life. These therapies aim to enhance mobility, alleviate pain, and promote overall well-being.
Physiotherapy for Arthritis:
Physiotherapy employs exercises, manual therapy, and modalities like heat and cold therapy to address arthritis. It aims to strengthen affected joints, enhance flexibility, and reduce pain. Techniques such as joint mobilization and tailored therapeutic exercises play a crucial role in enhancing joint function.
Osteopathy for Arthritis:
Osteopathy takes a holistic approach, focusing on the entire body to restore optimal joint and tissue function. Osteopathic treatments often involve gentle manipulations and adjustments to enhance joint mobility, reduce inflammation, and promote improved blood circulation. Osteopaths consider not only the affected joint but also surrounding muscles and tissues, providing a holistic arthritis management approach.
Enhancing Daily Living:
Beyond physiotherapy and osteopathy, arthritis management may include medications, lifestyle adjustments, and dietary modifications. Maintaining a healthy weight is vital, as excess weight can exacerbate joint stress. Assistive devices and joint protection techniques can also enhance daily functioning, allowing individuals to lead more fulfilling lives.
Conclusion:
Arthritis is a challenging condition, but it is manageable with the right approach. Physiotherapy and osteopathy are pivotal components of arthritis treatment, offering hope for improved mobility and enhanced quality of life. By comprehending the causes and symptoms of arthritis, exploring comprehensive treatment options, and addressing related diseases, individuals can take proactive steps toward a healthier, pain-free future.
For expert guidance and personalized arthritis treatment plans, consider consulting healthcare professionals at York Rehab Clinic. Our specialized team offers physiotherapy, osteopathy, and various services to address arthritis and related challenges. Your journey to arthritis management and improved well-being begins here.