The lumbar spine can be affected by various conditions that might seem confusing due to their similar names. This article will clarify the differences between spondylolysis, spondylolisthesis, spondylitis, and spondylosis.
Spondylolysis (Pars Interarticularis Defect)
Spondylolysis is an anatomic defect or fracture in the pars interarticularis, a part of the vertebral arch, commonly occurring in the lower lumbar spine, particularly at the L5 vertebra. This condition affects about 5% of the population and is not present at birth but develops over time, potentially running in families. It is often caused by repetitive trauma, especially hyperextension, which can lead to stress fractures. While spondylolysis is generally asymptomatic, some patients may experience activity-related low back pain or hamstring tightness.
Diagnosis typically involves imaging studies. AP and lateral X-rays can detect defects in about 80% of cases, showing the defect with or without sclerosis. Oblique views may add another 15% to the diagnosis. The “Scotty dog” sign refers to the normal appearance of the lumbar spine when seen on oblique radiographic projection. If spondylolysis is present, the pars interarticularis, or the dog’s neck, will have a defect or break (as if the dog has a collar around the neck). A CT scan is the best method to check for healing, while a SPECT scan is useful when X-rays are negative, but suspicion remains high. On X-rays, the condition appears as a radiolucent gap.
Treatment for spondylolysis generally includes rest, physical therapy, and activity modification to avoid hyperextension, with bracing used in some cases. Surgery, such as pars repair or spinal fusion, is considered if conservative treatments fail or if the condition progresses to spondylolisthesis. Many cases can fully heal with appropriate early treatment, allowing patients to return to normal activities, although some may experience chronic pain or require ongoing management or surgery.

Spondylolisthesis (Vertebral Slippage)
Spondylolisthesis occurs when a vertebra shifts out of place, typically due to a stress fracture that weakens the bone and compromises its proper positioning. This forward slippage of the vertebra, not to be confused with a disc slipping, can affect the nerves. An example of this is the Hangman’s fracture (slippage of C2-C3). About 15% of patients with pars defects progress to forward slippage. In pediatric cases, L5-S1 slippage occurs in 90% of instances, while L4-L5 slippage, usually degenerative, commonly affects adult females.
Types of spondylolisthesis include:
- Congenital
- Isthmic: The most common type, usually resulting from a pars defect at L5.
- Degenerative: Arising from facet arthritis, it predominantly affects females over 50 years and African Americans, typically at the L4-L5 level. The slip is generally mild and rarely exceeds 30%, but it is often associated with instability and lumbar stenosis. Flexion-extension X-ray views are sometimes needed to assess instability.
- Other Rare Types: Traumatic, pathologic, and post-surgical.
Spondylolisthesis is graded based on the degree of slippage:
- Type I: Less than 35%
- Type II: 25–50%
- Type III: 50–75%
- Type IV: 75–100%
- Type V: Spondyloptosis
Lateral view X-rays are used to measure the grade and slip angle, with the pelvic incidence calculated as the sum of the pelvic tilt and sacral slope.
Surgical considerations vary by location and severity of slippage. For L1-L4, repairing the defect is considered if conservative treatments fail. For L5-S1, in situ fusion is recommended for lower grades, while high-grade isthmic slippage may require fusion from L4-S1. Reducing the slip in such cases may risk L5 nerve root injury.

Spondylitis (Vertebral Inflammation)
Spondylitis is an inflammation of the vertebrae that can affect either the lower spine or the cervical spine. It may also lead to an epidural hematoma, necessitating a laminectomy and posterior spine fusion.
Examination
- Pott’s Disease (TB of the spine): Pott’s disease is tuberculosis of the spine, leading to severe vertebral damage and deformity.
- Ankylosing Spondylitis: This is an autoimmune disease that affects the spine and sacroiliac joints, progressing from inflammation to fusion. A characteristic radiographic feature is the “bamboo spine,” caused by the fusion of vertebral bodies through marginal syndesmophytes. The HLA-B27 genetic marker is positive in the majority of cases.
- Fractures in Ankylosing Spondylitis: Fractures may be hidden (occult) and require a CT scan or MRI for diagnosis. Care must be taken to avoid neurological injury during the examination and diagnosis proces

Spondylosis (Vertebral Arthritis)
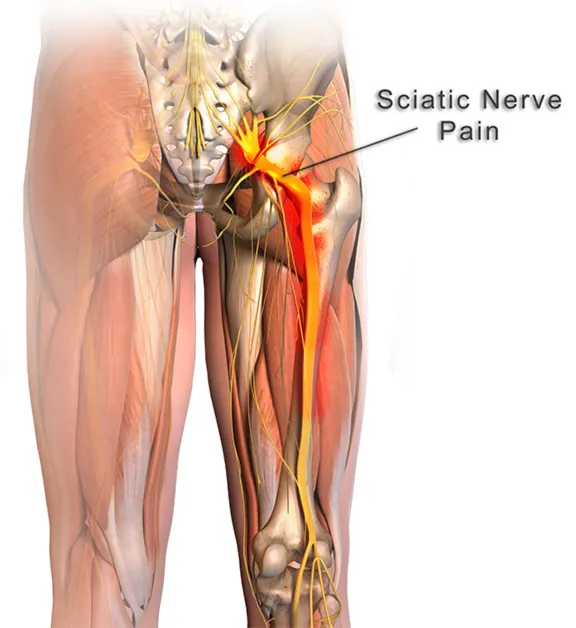
Spondylosis, often referred to as vertebral arthritis, is a degenerative condition affecting the joints between the vertebrae and the neural foramina. Over time, the degeneration leads to a narrowing of the space between adjacent vertebrae, resulting in compression of the nerve roots. This compression manifests as radiculopathy, characterized by pain, sensory disturbances, and motor changes.
In the cervical spine, where the condition is particularly prevalent, the compression caused by arthritis can extend to the spinal cord, leading to a condition known as myelopathy. Myelopathy can cause a variety of symptoms, including weakness, numbness, and difficulties with coordination and balance. As spondylosis progresses, it can significantly impact an individual’s mobility and overall quality of life.Spondylosis (Vertebral Arthritis)
Spondylosis, often referred to as vertebral arthritis, is a degenerative condition affecting the joints between the vertebrae and the neural foramina. Over time, the degeneration leads to a narrowing of the space between adjacent vertebrae, resulting in compression of the nerve roots. This compression manifests as radiculopathy, characterized by pain, sensory disturbances, and motor changes.
In the cervical spine, where the condition is particularly prevalent, the compression caused by arthritis can extend to the spinal cord, leading to a condition known as myelopathy. Myelopathy can cause a variety of symptoms, including weakness, numbness, and difficulties with coordination and balance. As spondylosis progresses, it can significantly impact an individual’s mobility and overall quality of life.

Conclusion
Understanding the differences between spondylolysis, spondylolisthesis, spondylitis, and spondylosis is crucial for proper diagnosis and treatment. Each condition has distinct causes, symptoms, and treatment options, underscoring the importance of targeted medical approaches for effective management and improved quality of life.